Posted by - admin \
May 29, 2023 \
Filed in - Health \
HMPV Human metapneumovirus lower respiratory illness \
3.8K views \ 0 reviews
DLNews Health:
While the flu season has passed and weekly COVID-19 diagnoses are declining, another respiratory virus is a rising threat. Known as human metapneumovirus (HMPV), it can cause upper and lower respiratory illness.
Many of the illnesses caused by it are severe, especially for infants and older adults who may have underlying conditions. Its peak time is winter and spring when RSV and influenza are circulating.
What is HMPV?
Human metapneumovirus, or HMPV, is a virus that causes respiratory infections in children. It was discovered in 2001 and is closely related to the respiratory syncytial virus (RSV).
Studies have shown that HMPV circulates each year predictably, peaking in winter and sometimes into spring. Like RSV, HMPV typically causes lower respiratory tract illnesses like bronchitis and pneumonia. In most cases, hMPV symptoms can be treated at home with plenty of fluids and pain relief. However, in some people, especially those under age five and over 65, hMPV can cause more severe complications that require medical attention.
Although HMPV is common, doctors don’t often test for it. That’s partly because a positive result wouldn’t change the care they give patients. It's also somewhat because hMPV differs from the viruses that healthcare professionals commonly test for, such as RSV and influenza. Its closest recent ancestor is a bird virus, making it an example of zoonosis: an animal pathogen that jumps to humans.
How do I get HMPV?
Infection with HMPV is spread by close contact with someone infected, usually through coughing or sneezing, which sprays droplets containing the virus into the air and onto nearby surfaces. The virus can also live on materials, such as tables, handrails, doorknobs, toys, and other objects, and people who touch contaminated items can then transfer the infection to their eyes, nose, or mouth.
Typically, HMPV results in a cold-like illness that goes away in a few days. But it can lead to more serious respiratory infections in children and adults with weakened immune systems. These include bronchiolitis, pneumonia, and acute exacerbations of chronic lung diseases like asthma and chronic obstructive pulmonary disease (COPD).
Discovered in 2001, HMPV belongs to the paramyxoviridae family with other viruses that cause respiratory infections, such as measles, mumps, and RSV. However, HMPV is distinct from its cousin in that it doesn't use the exact mechanism to overcome immunity that RSV does.
What are the symptoms of HMPV?
Most people will get a cough and runny nose when they have HMPV, but it can also lead to more severe symptoms like breathing difficulties. Kids and adults with underlying extreme conditions must immediately see their doctor.
The most common sign of HMPV is upper respiratory symptoms like cough, stuffy or runny nose, and congestion. But it can also cause lower respiratory symptoms like bronchiolitis, croup, and pneumonia in children. It can also trigger acute asthma exacerbations in adults.
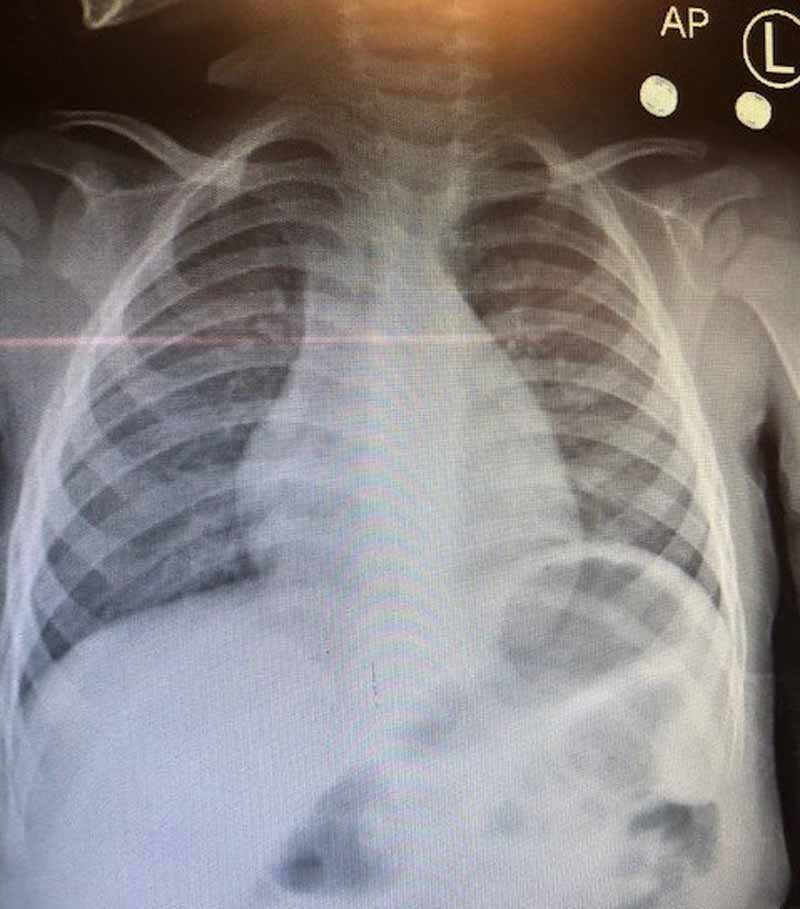
Most people recover at home with over-the-counter drugs like cough syrups, decongestants, and pain relievers/fever reducers (like ibuprofen or acetaminophen). But in very severe cases, a healthcare provider might do a bronchoscopy to insert a tube with a camera into the lungs to get a fluid sample. It can help doctors figure out if HMPV is the cause of the problem. HMPV usually circulates in winter and spring but is more active than usual this year.
What are the risks of HMPV?
Acute infections caused by HMPV usually last about a week and are mild. HMPV circulates predictably every winter and spring, peaking in February through May in North America. Unlike RSV and influenza, healthcare providers don't typically test for HMPV in people who come to their offices with suspected infections.
Instead, they rely on symptoms and family health history to diagnose. They don't have specific antiviral drugs for hMPV, but they can help manage symptoms and complications like bronchiolitis and pneumonia.
HMPV is believed to have jumped from a bird virus, avian metapneumovirus (AMPV), and evolved into its present form in humans. Research suggests that hematological conditions such as chronic lymphocytic leukemia (CLL) may contribute to more severe courses of infection and a higher risk of death in older adults. Intensive care hospitalizations and fatal cases of pneumonia have been reported in HMPV-infected patients. Acute conditions tend to be more common in children and younger adults.
A 2020 study in the Lancet Global Health estimated that children younger than 5 had more than 16 million HMPV infections in 2018, more than 600,000 hospitalizations, and more than 16,000 deaths.

Desert Local News is an invitation-only, members-based publication built on fact-checked, non-biased journalism.
All articles are publicly visible and free to read, but participation is reserved for members—comments and discussion require an invitation to join.
We cover local, state, and world news with clarity and context, free from political agendas, outrage, or misinformation.
Comments